Subperiosteal bone grafting in implants is a bone grafting support method to fix and stabilize the jawbone area after surgery. A prerequisite for implant placement is that the jawbone must have sufficient thickness and quality. However, if the jawbone is severely resorbed, a subperiosteal implant becomes the optimal treatment solution, helping to restore chewing function and aesthetics for the patient.
What is a Subperiosteal Implant?
Subperiosteal implants are a dental implant method dating back to the 1940s. However, the history of subperiosteal implants recorded a success rate of only about 30–40% at that time. Thanks to the outstanding advancements in modern technology, the success rate has now increased to 97–98%.
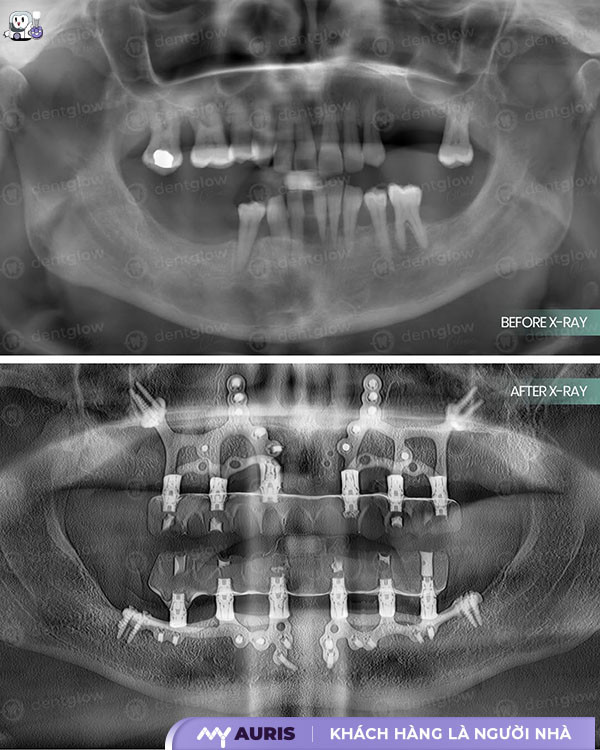
The improvement comes from the application of many advanced technologies such as CT Cone Beam systems, 3D X-rays, 3Shape 3D digital impression devices, 3D facial scanning technology, combined with modern digital equipment and supporting software. As a result, the process of fabricating personalized implants has become faster and more accurate than ever before.
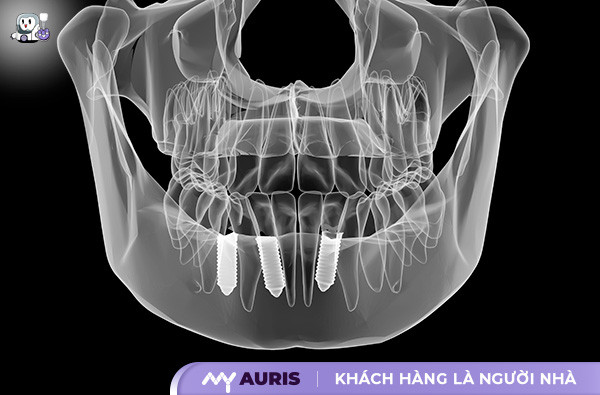
Unlike conventional implant placement, which inserts the implant post deep into the jawbone to replace the natural tooth root, the subperiosteal implant method uses a metal framework placed between the jawbone and the gum, specifically beneath the periosteum—a thin layer of tissue located between the gum and the bone.
The special feature is that the tooth root post in this technique is not embedded *into* the bone but placed *on* the bone, beneath the gum tissue. This eliminates barriers related to jawbone density or shape, while still ensuring effective osseointegration.
After integration, the prosthetic teeth are attached to a stable foundation, creating a natural feel and long-term stability. Patients will not have to worry about teeth shifting or slipping out of place, as with non-standard traditional methods.
A notable advantage of this technique is that the healing time is often faster than traditional implants, although the surgical time for both methods is almost equivalent.
When to Consider Subperiosteal Implant Placement?
Subperiosteal implant placement is an optimal choice for individuals suffering from jawbone resorption, complete tooth loss, or loss of most posterior teeth, especially when the jawbone conditions are insufficient for conventional implant placement.
This method is also indicated in cases of bone loss due to thyroid issues, calcium deficiency, old age, or hereditary jawbone deficiency. It is an effective dental restoration solution, helping to restore chewing function and aesthetics.
Furthermore, patients who have undergone jawbone resection due to cancer, those with osteonecrosis of the jaw, congenital anodontia (born without teeth), or previous failed implant placements are also suitable candidates for this implant technique. In situations where the jawbone is shallow, making conventional implant placement unfeasible, subperiosteal implants offer a reliable alternative.
However, to determine whether you are an ideal candidate for subperiosteal implant placement, it is crucial to consult with a specialist dentist to choose the most suitable and safest restoration solution.

Comparing Subperiosteal Implant Technique and Traditional Implants
Both subperiosteal implants and traditional implants are effective solutions for tooth loss restoration. However, each technique has its own characteristics regarding implant placement, structure, indications, and procedure, suiting specific jawbone and gum tissue conditions, as well as treatment needs.
Regarding Implant Placement Location
Traditional Implants: The implant post is placed directly into the jawbone, acting as an artificial tooth root, providing high stability.
Subperiosteal Implants: The implant post is placed between the gum tissue and the jawbone, just beneath the periosteum, not deeply into the bone like traditional techniques.
Regarding Implant Indications
Traditional Implants: Suitable for most cases of single tooth loss, multiple tooth loss, or full arch tooth loss, provided the patient has sufficient quantity and quality of jawbone to secure the implant post.
Subperiosteal Implants: An optimal solution for cases of severe bone resorption, overly thin jawbones, where traditional methods cannot be applied. Particularly effective for patients with:
- Jawbone resection due to cancer
- Osteonecrosis of the jaw
- Congenital anodontia (born without teeth)
- Elderly patients with multiple underlying conditions who cannot undergo bone grafting
- Previous failed implant placements
Regarding Implant Structure
Traditional Implants: Consists of 3 basic parts – the implant post, the abutment, and the prosthetic tooth attached to the post.
Subperiosteal Implants: Composed of 2 parts – a metal framework secured to the bone with screws, and a post extending into the oral cavity for prosthetic tooth attachment.
Regarding Implant Placement Technique
Traditional Implants: The procedure is highly invasive, involving the following steps:
- Gum incision
- Jawbone drilling
- Implant post placement
- Gum suturing
- Waiting for osseointegration
- Attaching the permanent prosthetic tooth
If necessary, patients may also need to undergo additional procedures such as sinus lifts or bone grafting to ensure suitable conditions for implant placement.
Subperiosteal Implants:
- Making a small incision in the gum
- Drilling the gum tissue and placing the metal framework onto the bone
- Suturing the gum and waiting for healing
- Attaching the posts to the framework, waiting for integration, and then proceeding with tooth restoration.
Regarding Popularity
Traditional Implants: This is a common technique in most dental clinics and Maxillofacial Hospitals, widely applied with a high success rate.
Subperiosteal Implants: Introduced in 1940, it remains rare today due to a lower success rate and high demands on surgical skill, posing a significant challenge for dentists during treatment.
Should You Choose Subperiosteal Implants or Traditional Implants?
In the field of tooth loss restoration, traditional implant placement is always the preferred choice if the patient has a healthy jawbone. This method facilitates easier implant post placement, resulting in a high success rate and quick recovery.
However, for cases with insufficient bone, dentists often recommend additional procedures such as sinus lifts or bone grafting to regenerate bone, creating a solid foundation for implant placement.
In severe situations such as severe bone resorption, when traditional implants or zygomatic implants cannot be applied, subperiosteal implant placement is the ideal solution. Although the technique is more complex, this method still effectively restores lost teeth, providing stable chewing function and an aesthetic smile for patients.
Regardless of the technique chosen, visiting a reputable dental clinic for accurate consultation is extremely important. Only a highly qualified dentist can determine the most suitable solution for each patient’s jawbone condition and needs.
Is Dental Bone Grafting Painful?
The alveolar bone grafting process is completely painless thanks to skilled dentists, local anesthesia, and support from modern equipment and technology. This technique creates artificial jawbone to replace resorbed bone, providing stable support for dental implant placement.
How Long Does Dental Bone Grafting Take to Heal?
The healing time after dental bone grafting depends on each individual’s body, typically taking about 2–6 months for the jawbone to recover. Afterward, the dentist will assess the jawbone condition and formulate the next treatment plan.

Post-Surgery Care Instructions
After subperiosteal implant surgery, each individual will have a different recovery rate. However, mild to moderate pain in the surgical area is common during the first few days. To manage this, the dentist will prescribe pain relievers and antibiotics. Adhering strictly to the medication regimen will optimize the healing process.
Another important factor to note is smoking. This is a leading cause of increased risk of restoration failure. Therefore, patients should stop smoking at least 2–4 weeks before and after surgery to ensure the success of the treatment.
Jaw swelling is also a common reaction after the procedure. To reduce swelling and pain, patients should apply an ice pack to the cheek area for 15–20 minutes at a time, during the first 24–48 hours.
In the first few days after surgery, prioritize rest and avoid strenuous physical activity to facilitate wound healing. Regarding diet, patients should choose soft, liquid foods and avoid hard, oily, crispy, or crumbly foods, as they can affect the implant site.
Proper oral hygiene is vital during the recovery phase. Use antibacterial mouthwash as directed to keep the oral cavity clean, prevent bacterial invasion, and avoid infection.
In summary, subperiosteal implant placement is an advanced tooth restoration solution, especially suitable for cases of tooth loss, congenital anodontia, or severe jawbone resorption—conditions that traditional implant techniques cannot address. With proper care, patients can fully expect a quick recovery and lasting restoration results.





